Batch Claims Claims with Issues
Batch Claiming
Directors (and Plan Managers with elevated Claim permissions) are now able to submit claims to NDIS in a Batch. This has been introduced to enable the submission of claims beyond 90 days after a plan has ended.
Some agencies who also use a review process prior to submitting all claims may find this feature useful. However, Agencies should note that direct visibility of any real time issues is lost when using this process. To counter this, any claim with a claim line either rejected or with an exception raised will go into Claims With Issues listing as it will need to be reviewed.
Plan Managers without elevated claim permissions can indicate that a claim is finalised and ready to claim via a batch submission, but they are restricted from selecting batch ready claims and submitting.
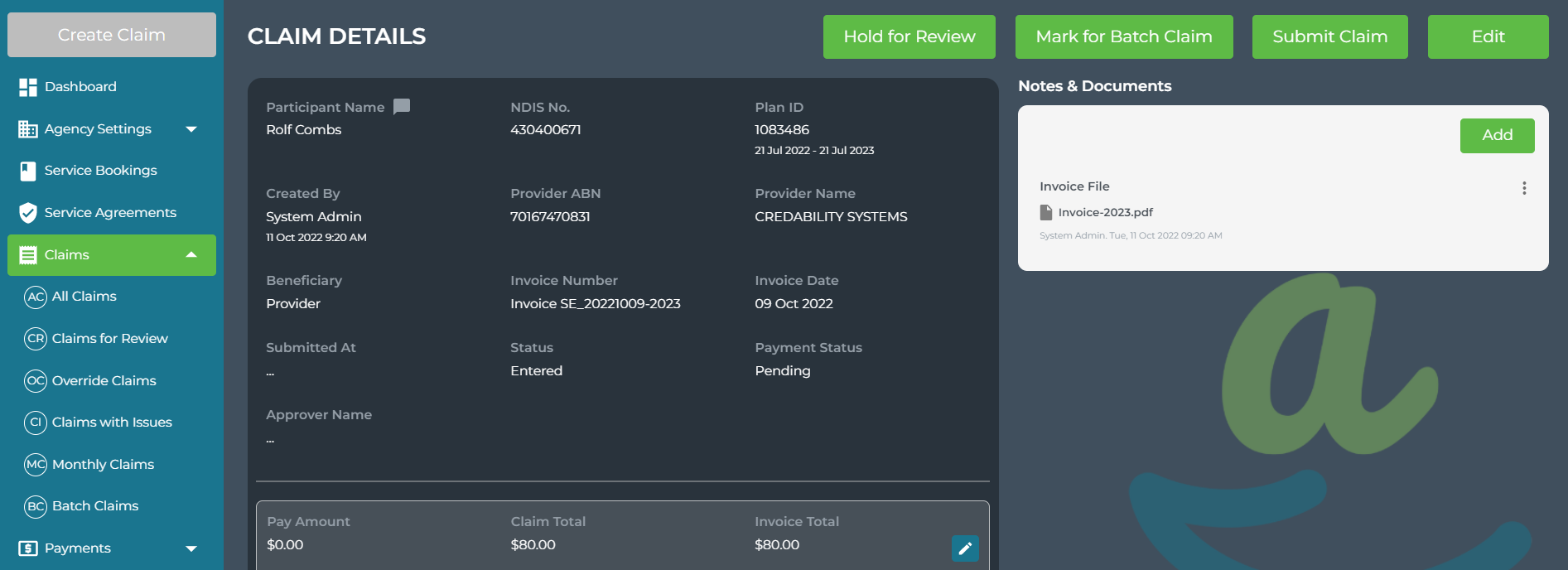
Any claim that is Marked ready for Batch Claim can still be submitted individually (except those older than 90 days from the Service Booking end date).
Claims that are Held for Review cannot be Marked ready for Batch claim. They will have to be Marked as Reviewed and then either submitted to NDIS or Marked for Batch Claim.
To create a batch of claims to submit to NDIS:
From Claims > Batch Claims, select the claims to be included in the batch. Use the filter or search options to refine your listing if required.
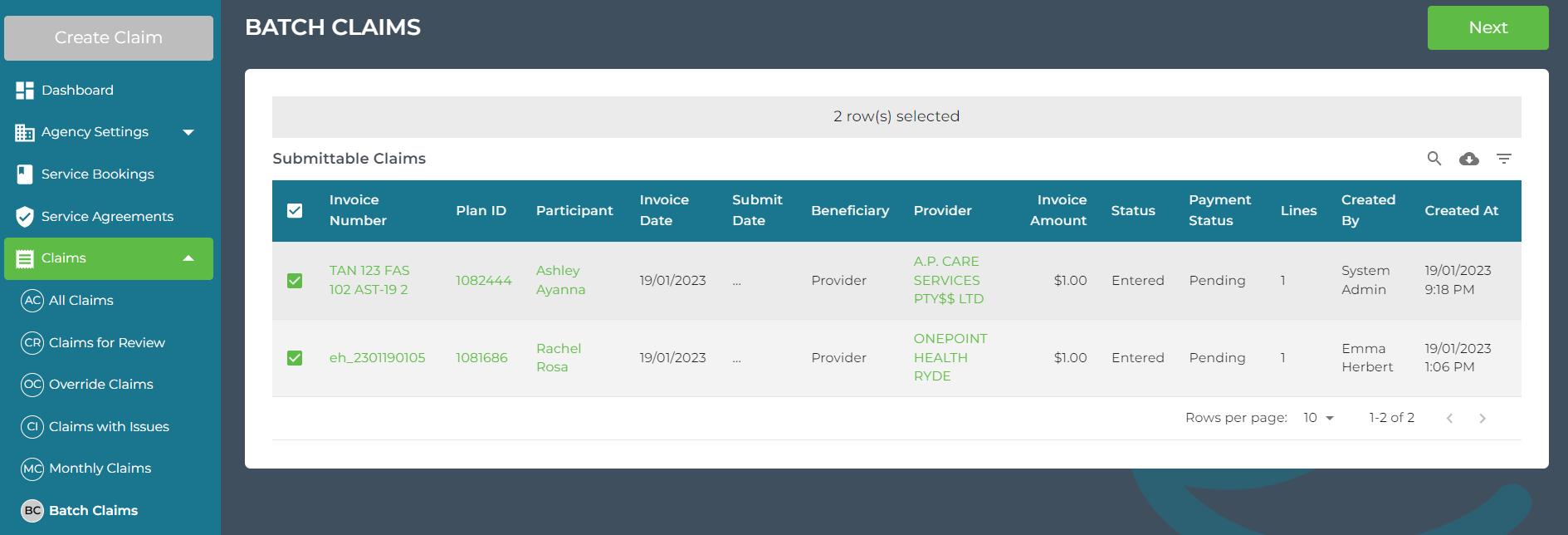
Click Next to continue
You can remove claims from the batch by clicking on the ![]() icon to the left of the Invoice number.
icon to the left of the Invoice number.
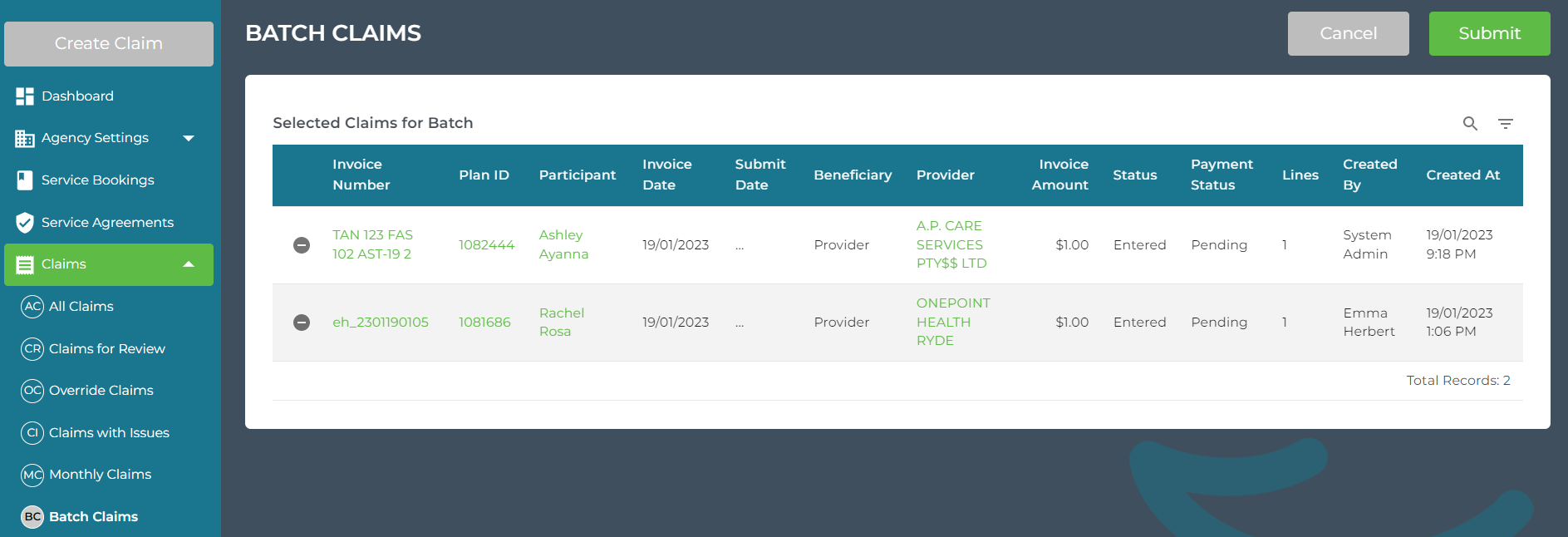
Submit the Batch to NDIS by clicking Submit, you will see a confirmation that the batch has been submitted:
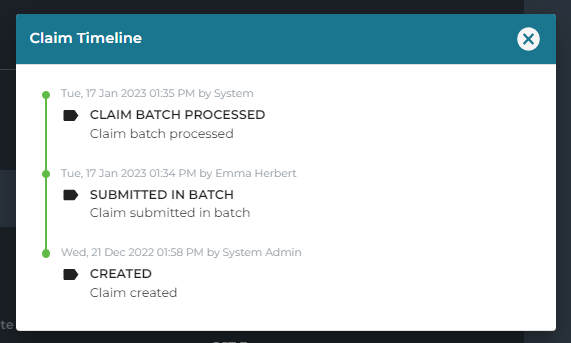
The Claim timeline will show the time the claim was submitted in Batch and the time the claim was Processed.
Claims with Issues list
We have introduced a new view under Claims - Claims with Issues.
This will identify any claim with an issue that needs to be addressed. These are claims that are in an approved or entered status that have:
- at least one rejected claim line;
- and/or at least one claim line where an exception was raised by NDIS which has prevented the provision of a PRN.
If the response from NDIS to a submitted claim is either a rejection or an exception, the claim will be displayed in the list until the issue has been rectified.
We anticipate this may occur if an error happens and is not noticed at the time of submission; or when a carer/participant approves a claim; or when the claim is part of a batch claim.
Claims with Issues is different to Override claims. Override Claims holds claims that have a rejected or cancelled claim line. They need to be checked and updated and/or payment enabled.
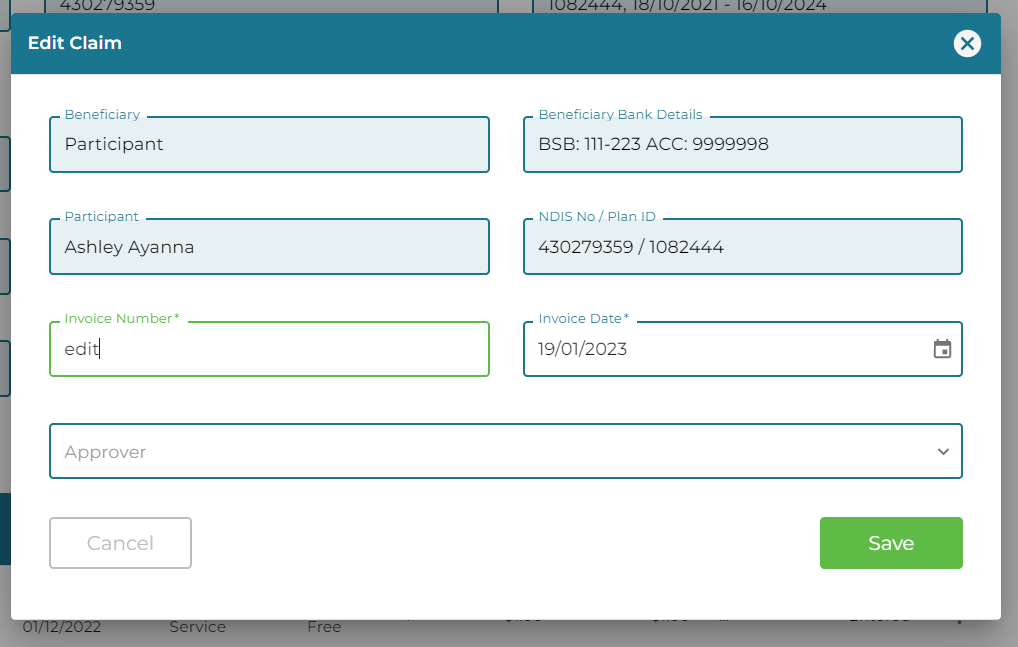
Edit the invoice number of participant reimbursements
We have allowed manual entry of Participant Reimbursement invoice numbers. If this field is left blank we will generate one automatically using their NDIS number and date and time to ensure they are submitted with a unique invoice number in the format: NDISNumber-YYYYMMDD-HHMMSS
eg: 430399604-20230117-174953
The Invoice number is also now an editable field from Edit Claim.
Enter BPay Reference on Claim
We have added a BPay Reference field to help streamline the Payment process. When entering a claim for a Provider that has BPay selected as the default payment setting you will be required to enter the BPay Reference.
We have removed the BPay Reference field on the Provider Details page.
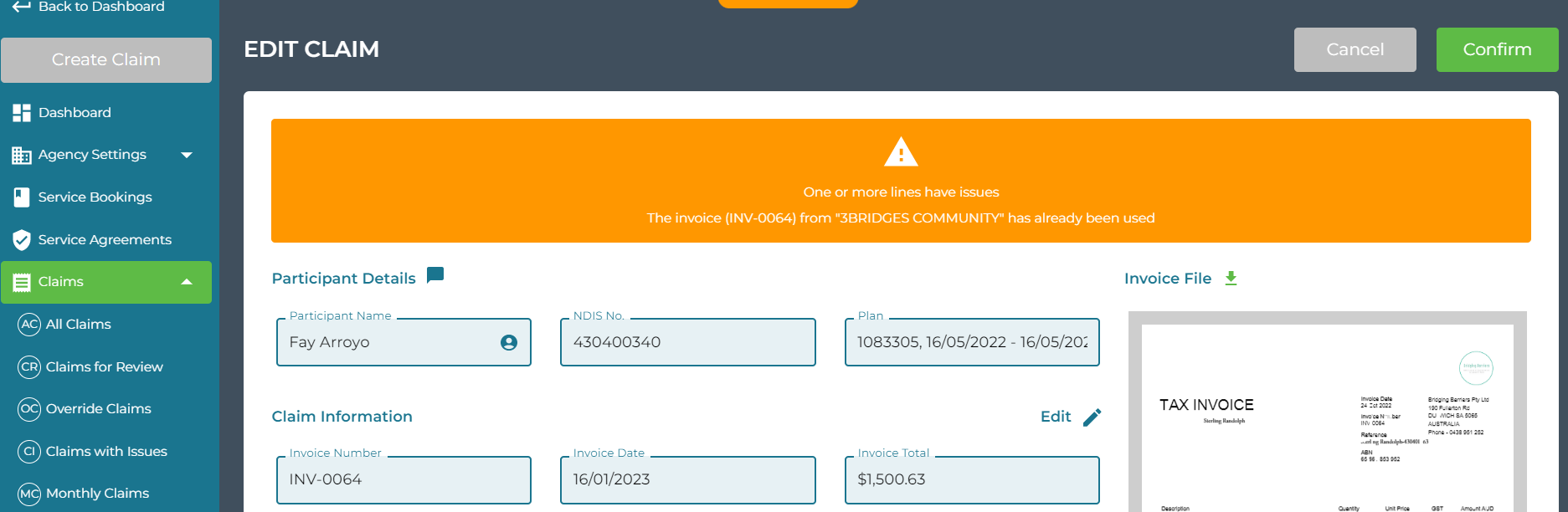
Duplicate Invoice Warning/Block Amendment
It is not possible to manually enter a claim with an invoice number that has already been entered for the same Provider.
However, if the claim has been scanned the claim will still create in Planabilty for you to review. We are making it very clear on both the Claim Details page and on the Edit Claim page that the Invoice number has already been used.
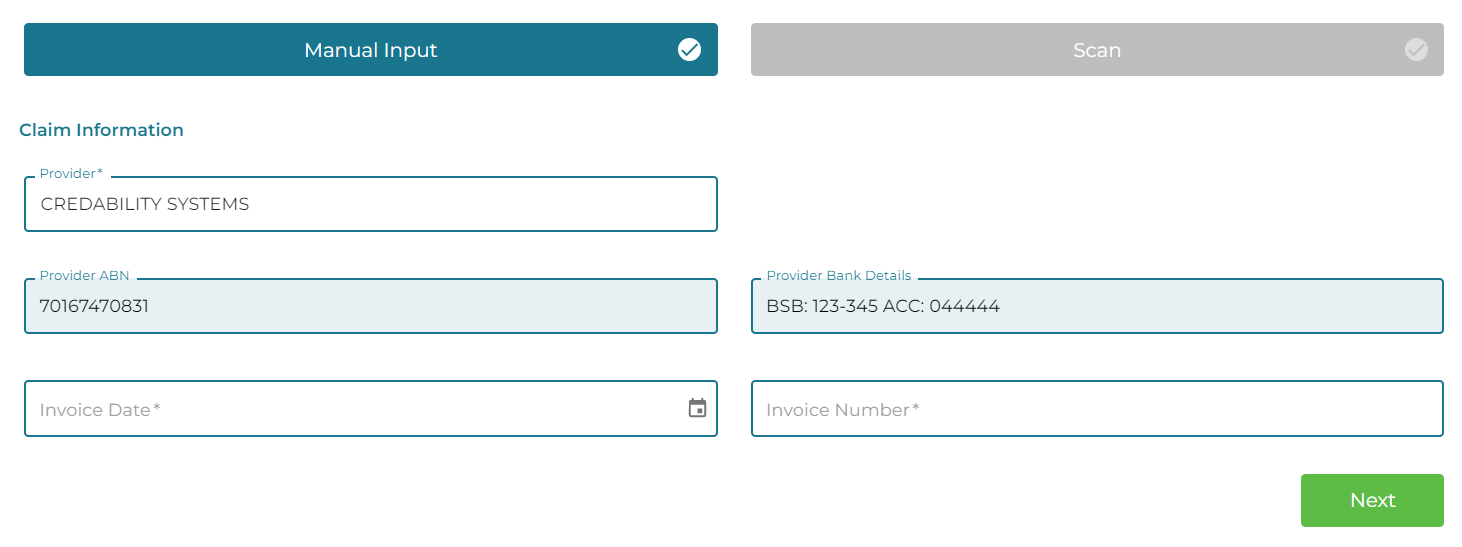
ABN Displayed in Provider field when creating claim
Both the Provider ABN and Bank Details are now displayed when creating a claim. Select the Provider by entering the Provider name or ABN in the Provider field.
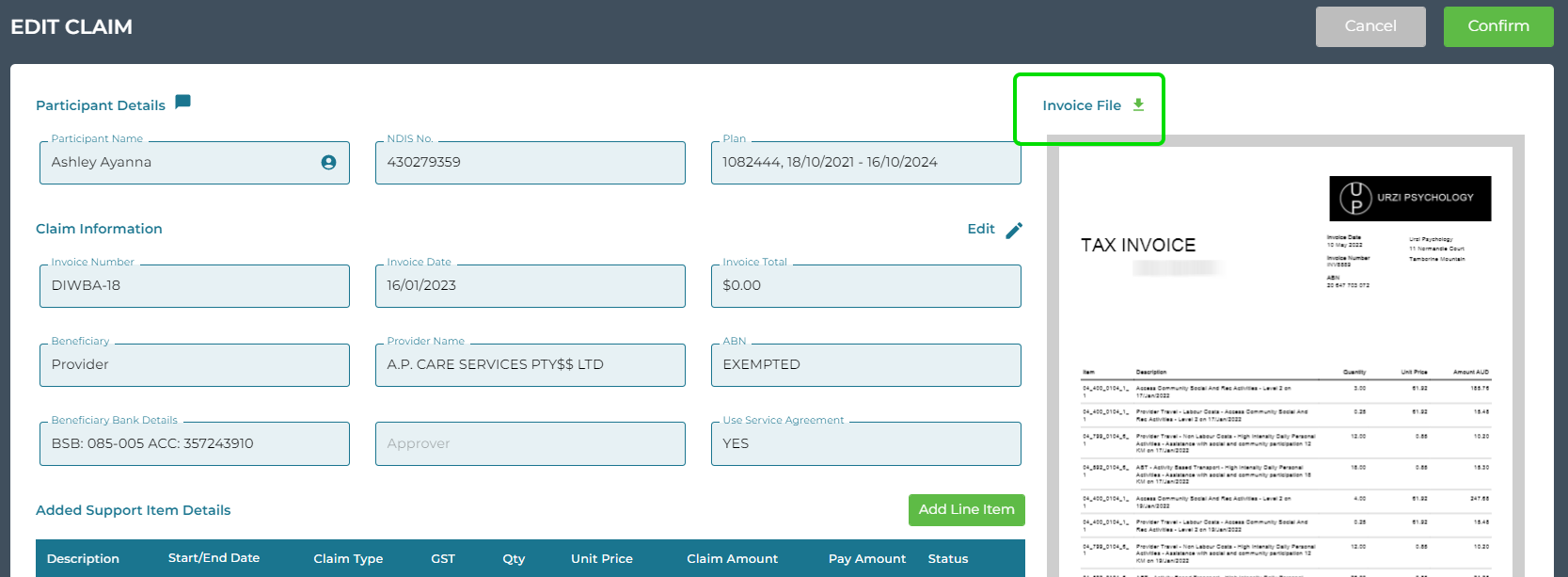
Download the Invoice file from the Edit Claim screen
The Edit Claim page now includes a link to download the Invoice File. When reviewing claims from Claims for Review or All Claims, use the right ellipses buttons to navigate directly to Edit. From the Edit Claim page you can view and update any potential line item errors, update the Claim Information (including selecting an Approver), and download the invoice file for easy viewing.
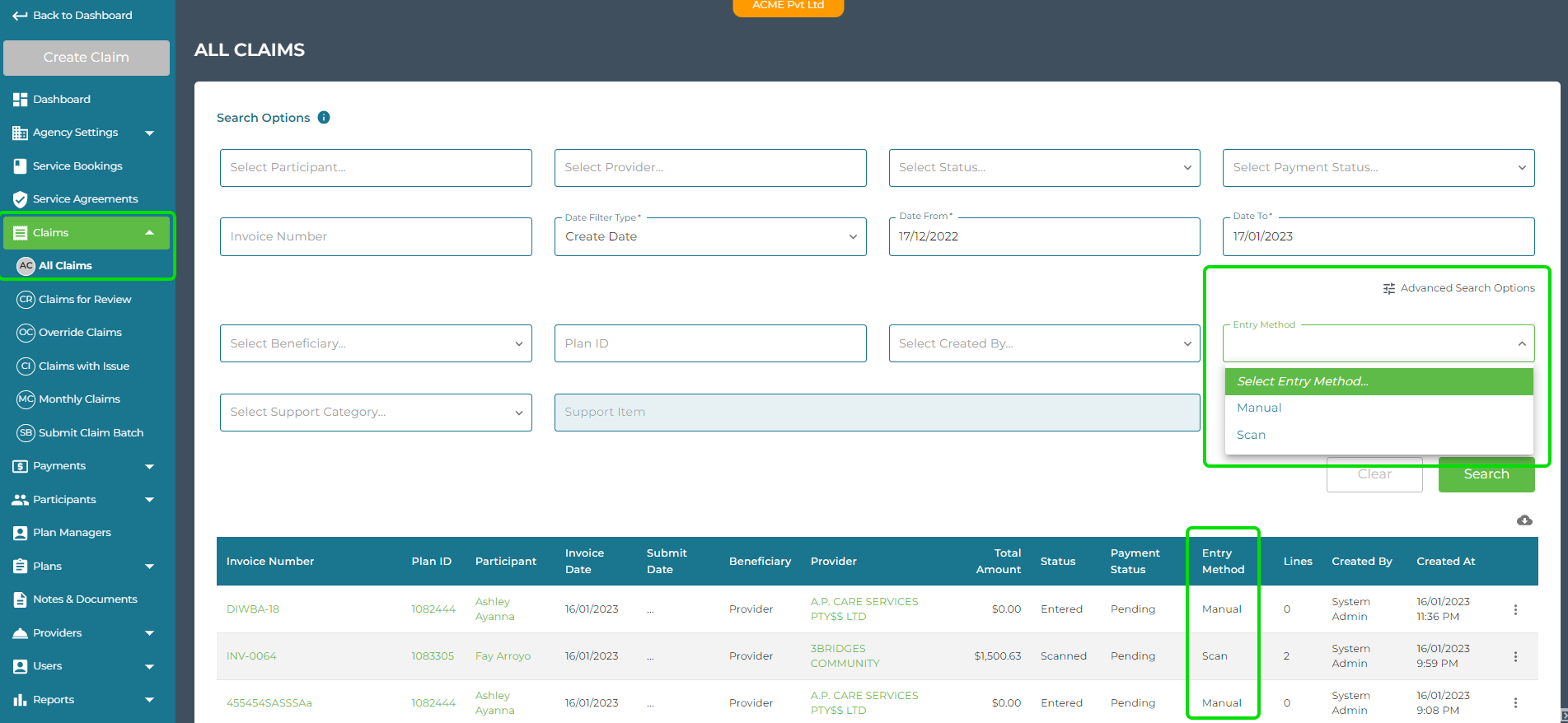
Identify the input method of claims
The All Claims listing now displays the claim entry method (Manual or Scan). Use the Advanced Search Options to refine your search by Entry Method.
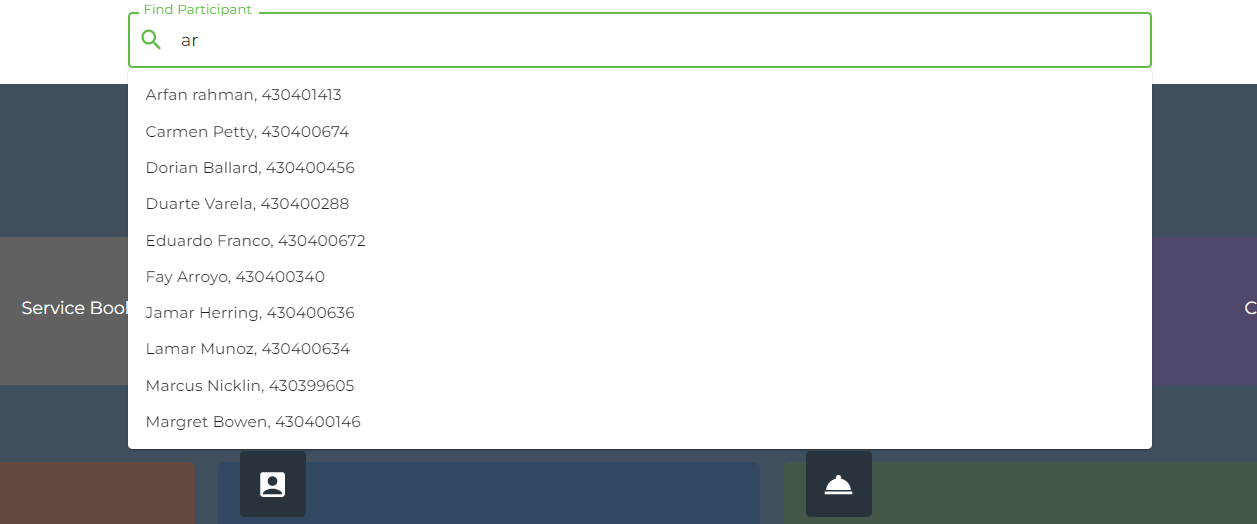
Participant and Provider suggestions
We have increased the number of suggestions displayed when selecting a Participant or a Provider. After a 2nd character is entered, we now show up to 10 suggestions, the more characters entered, the more refined the suggestions will be.
Added Pagination to Create Batch Payments
We have added pagination to the Create Batch Payments view so that you can select to view 10, 50, 100, 250, 500, 750 or 1000 claims. This update will improve the loading time when selecting claims to add to Batch.
Select All will still select all claims that are payable, regardless of the number you are viewing per page. If viewing 10 per page, and 150 claims are ready for payment, Select All will select all 150 Claims.
Retained participant and plan selection view when creating claim
If creating a claim when drilled down to a Participant and Plan you will retain this perspective during the claim process. Previously you would lose the view of Participant and Plan in the left menu. We are keeping this visible so that you have easy access to their Claims and Service Bookings.
If scanning and you select to Scan Another, you will remain drilled down to that participant and plan ready to claim again for that participant.
If you claim from the main dashboard nothing is affected.
Fix: Generate Statement by Month (from Active Participants)
A permission issue was preventing some user types from generating the monthly statement. This has been fixed.
Note: if the monthly statement has already been generated you will not be able to generate it again, but you can access all generated monthly statements from the main left menu - Reports > Statements or from Participant and Plan menu - Statements.
Statements generated by date range are not saved but are downloaded to your device at the time of generation.
Fix: Generate Statement by Date Range on Previous Plan
We have published a fix to this feature so that you can now select a previous plan and date range. This will be useful for Plans that end mid-month and would not otherwise have had a statement generated automatically from the older Plan at month end.
Fix: Right hand side create buttons restored
Director users temporarily lost the Create button in the top right of the Active Provider listing and Claims listing at Participant and Plan level.
We know you missed that create option, so it has returned.
Enhancement: Date Picker
There has been an improvement made to the calendar date selection when creating a claim line. You can double click on a single date to select it as the Start and End Dates, previously the calendar dropped slightly for the end date selection. Sometimes this resulted in an earlier date being selected. The Calendar no longer drops which has made this a smoother process.
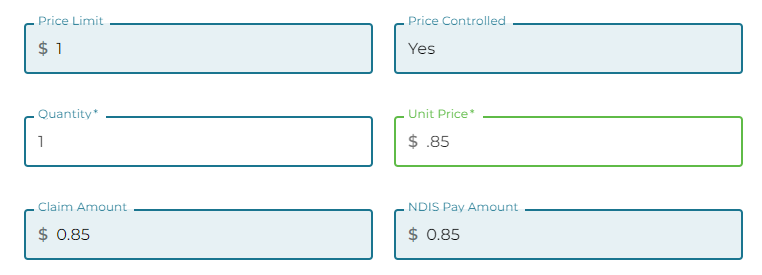
Enhancement: Unit Price
When adding a claim line, you can now enter the unit price below $1.00 without a preceeding 0.
eg: .85